 People often wonder why doctors aren’t more interested in apps for their patients, or in trying something new to help patients. After all, we expect doctors to care about their patients’ health.
People often wonder why doctors aren’t more interested in apps for their patients, or in trying something new to help patients. After all, we expect doctors to care about their patients’ health.
Plus, we know that doctors are now being held more accountable for outcomes, because we’re moving towards “pay-for-value.”
I do believe that most doctors care about their patient’s health. But it’s not easy being a PCP, and there are lots of reasons that the average PCP has difficulty optimizing the health of a medically complex senior.
Here is part III of the case study I created for my upcoming ebook: the point of view of Joan’s PCP, Dr. Miller. As you read, consider
- What’s the doctor focusing on when it comes to Joan’s health? How does that align with what Joan herself is most concerned about, and what her daughter is concerned about?
- What kinds of tools or services might help the PCP with what he’s trying to do for Joan’s health?
And for extra credit: what’s he overlooking that someone applying geriatrics — the art & science of modifying healthcare so it’s a better fit for older adults — probably would address? (Hint: it’s related to Joan’s vitals.)
Joan’s Health Story (According to Her Doctor)
Dr. Miller has seen twenty patients today already, back to back, and he’s running late again. He had to skip his lunch break to make up some time, and even so, he’ll be lucky if he finishes the day’s appointments by 5:30pm. He doesn’t want to stay any later than that, so he whisks through the next exam – a woman he sees every three months: 79-year-old Joan, diagnosed with COPD, atrial fibrillation, type 2 diabetes, hypertension, high cholesterol, depression, osteoarthritis, and chronic kidney disease. A pretty common combo of health problems, because hey, that’s what happens after a lifetime of smoking and being overweight.
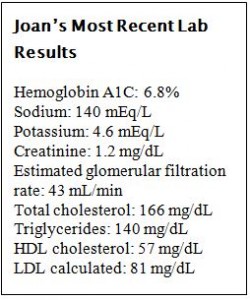 Dr. Miller skims through his last note and the key data assembled by his medical assistant. Hemoglobin A1C at goal? Check. Lipids under control? Check. BP at goal? Oh it’s 115/80 today, nice and low, very good. Pain? 5/10, as usual …presumably her arthritis pain. She also mentioned shortness of breath to the assistant, so he’ll need to figure out whether it’s her atrial fibrillation or her COPD acting up. Oh, and she reported a fall, but those are pretty common in people her age.
Dr. Miller skims through his last note and the key data assembled by his medical assistant. Hemoglobin A1C at goal? Check. Lipids under control? Check. BP at goal? Oh it’s 115/80 today, nice and low, very good. Pain? 5/10, as usual …presumably her arthritis pain. She also mentioned shortness of breath to the assistant, so he’ll need to figure out whether it’s her atrial fibrillation or her COPD acting up. Oh, and she reported a fall, but those are pretty common in people her age.
She’s asking about apps to help her mother manage her health care. Dr. Miller doesn’t really have time to explain to her the problem with apps – he has his hands full making sure all of Joan’s cardiovascular problems are on track – and besides, no app is built for someone like Joan. She’d need many apps covering multiple diseases, and anyway, in general older people don’t like using technology to track their health.In the room with Joan and her daughter Susie, he asks for more details about her breathing difficulties. He wants to find out if she’s been having palpitations, and if she’s been using her inhalers as directed, but Susie interrupts.
Susie can get argumentative, though, so he doesn’t explain, because he doesn’t have the time. Apps aren’t the way to go, he tells her. What’s most important, right now, if she wants to improve her mother’s everyday life, is her weight. If Susie can get her mother to eat a little better and exercise a little more – go for a 30-minute walk 4 times a week, for example – then she’ll be a lot better off.
Dr. Miller realizes he’s been in the room for 15 minutes already; time to wrap things up. He rattles off his recommendations: keep taking your medications, try to get more exercise, keep track of your pain, what you’re taking for it, and how you feel afterwards. He reminds them that exercise will help reduce fall risk and instructs his assistant to give Joan the clinic’s fall prevention tips handout.
As he leaves the room, Dr. Miller realizes that yet again, he hasn’t had a chance to check on Joan’s depression symptoms. Oh well, maybe at the next visit in three months. It’s tough, though, with all her other chronic problems that he needs to check on.
Dr. Miller isn’t a bad doctor. He wishes there was some better way to help Joan manage her health. She’s got a lot of diagnoses but he’s doing what he can to help her stay on top of things and he’s meeting the established quality measures for diabetes. They really should give him more time to meet with patients like her, though. Especially when family comes and has questions, it’s basically impossible to go in and out the door within 15 minutes.
He really can’t imagine an app helping her, although it would be nice to know what her pulse is when she gets short of breath. Maybe he’ll see if there are any good ones on the market. If he can find the time.
